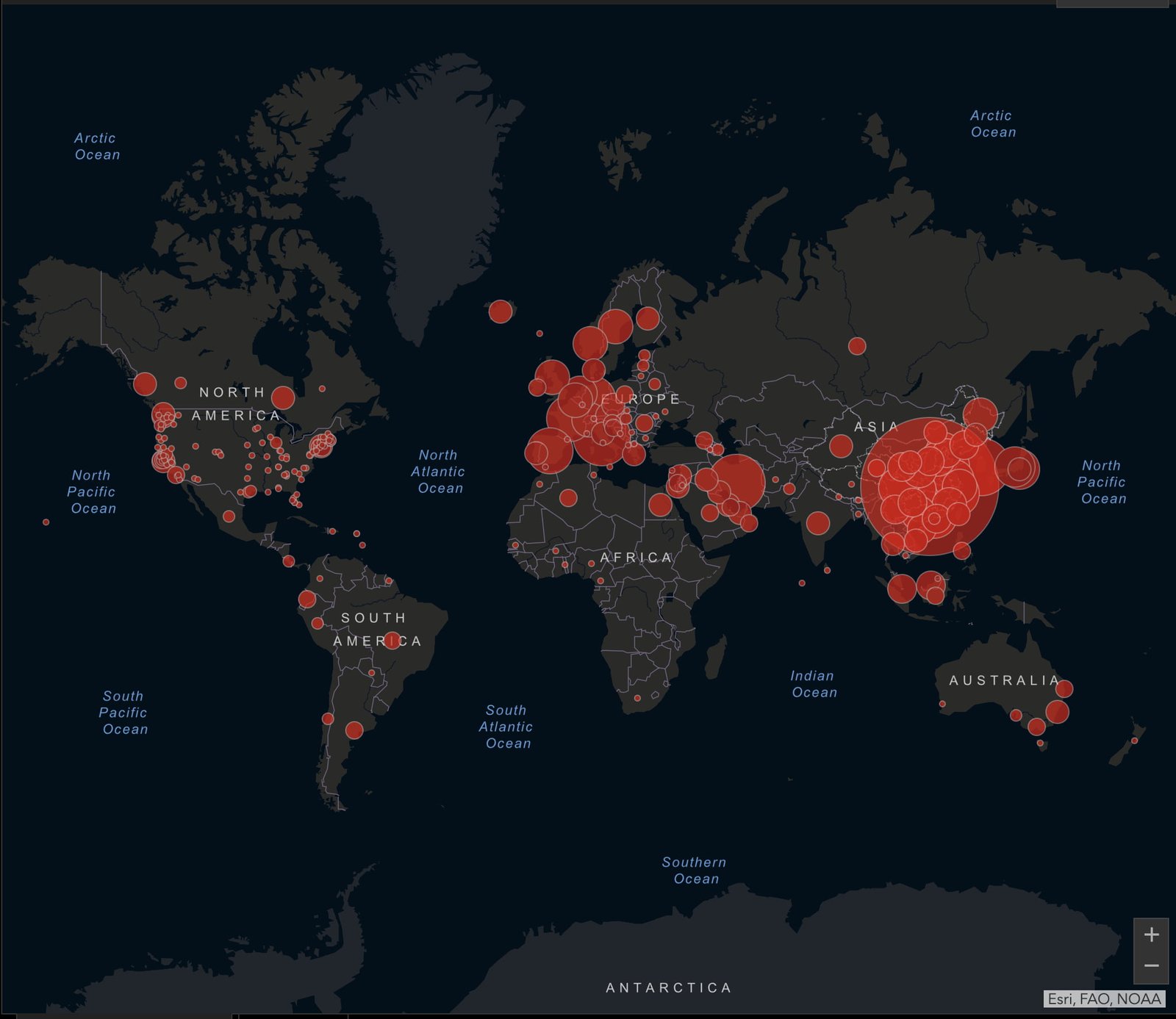
Fifteen nurses in quarantine, six of whom have tested positive for COVID
NASSAU, BAHAMAS — With 190 active cases of the coronavirus in Grand Bahama, healthcare professionals expressed concerns yesterday that the healthcare infrastructure on the island could be maxed out if an influx of patients require hospitalized care.
Bahamas Nurses Union (BNU) President Amancha Williams said while the majority of cases on the island remain in self-isolation “there is a serious problem”.
“If we add any more, and like Dr [Melisande] Bassett said, if we start to hospitalize — we have the Cancer Society, which is known as the CAB — we can only hold up to 16 patients,” said Williams, who appeared on ILTV’s ‘Beyond the Headlines’ with host Clint Watson.
“If these persons start to show respiratory symptoms what is going to happen?
“Tell me, what is the next plan? Do we open back up the tents? The tent situation we know on several occasions; just two weeks ago we had a deflated tent during an emergency surgery. Then a few weeks before we had to move the medical and surgical wards to the CAB.”
She said nurses await word on what will happen if an influx of patients required hospitalization in Grand Bahama.
She continued: “Can we handle this? No we cannot. What is the plan we are asking our government.”
As of July 23, there were 422 people in quarantine, according to Dr Frank Bartlett, head of the COVID-19 task force on Grand Bahama.
Of that figure, he said 111 were isolating at home, 20 were quarantining at a government facility and 11 were isolated at a government quarantine facility.
Grand Bahama remains on a two-week lockdown until August 7 at 5am to curb the spread of the virus.
Bahamas Doctors Union President Dr Melisande Bassett said once capacity has been reached there is nothing else that can be done.
She said the conversion of the South Beach Clinic to a negative pressure facility with more beds was an innovative move, but options must be explored to source additional capacity, and quickly.

“Heaven forbid we experience an inadvertent exposure like we did the last time,” she said, referring to a hospital exposure where over 200 healthcare professionals had to be tested.
“I don’t think we would be able to sustain the level that we’re at and even more with shortages for very long, so we need the physicians back in hospital.”
She said her greatest concern remains preservation of life.
Meanwhile, Dr. Sabriquet Pinder-Butler, president of the Consultant Physicians Staff Association (CPSA), predicted that among the influx will be patients who require greater care.
“With the exponential increase in numbers, we anticipate that we will see, more than likely, more persons coming in that are high-risk and that need care, that will have moderate of severe cases of COVID-19,” she said.
Tough calls
According to Pinder-Butler, physicians continued to work under pressured conditions, with tough calls to make everyday that could affect patient outcomes.
“On a day to day basis, sometimes you are trying to make a call as to making sure you stratify who may be the [most] ill patient for example, and who requires the bed soonest; who can be shifted out; if we can swap out patients from one area to the next just to make these things happen,” Pinder-Butler said.

“That happens and sure it is happening now, so certainly the physicians are concerned because again we are seeing increases in the capacity of patients with COVID.
“We know that there are patients with chronic conditions who also need care; emergencies will continue to happen.
“These are everyday things that we deal with on a daily basis, so you know, it’s a difficult when you may have one bed left and you have two very ill patients…”
Pinder-Butler said test results still require two to three days to turnaround, and the timeframe is another variable that can strain available resources.
She again called on the government to meet with the CPSA to better work together and be apprised on how physicians and the wider public will be kept safe.
At risk
Williams said while nurses remain resilient, “it is not easy” with 15 nurses in quarantine, six of whom she said tested positively for the virus.
As of yesterday, there were 382 confirmed cases of COVID-19 in The Bahamas.
An additional 40 new infections were confirmed on Monday.
“This leaves the nurses in a position where they are overly worked and here again, I am always going to say this, underpaid,” she said.
“When you have a institution as Freeport, the Rand Memorial, and we see what is happening there. You have an A&E (Accident and Emergency) Department that is in the foyer sharing bed space and also triaging new patients in. Then we say to this government, we are in a serious position.”